What is Pleural Effusion?
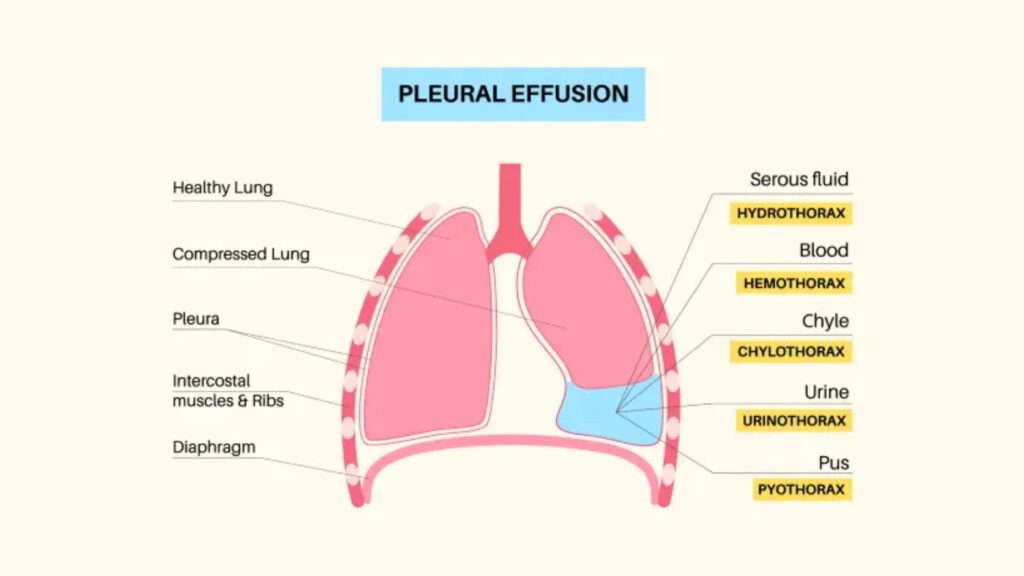
Pleural effusion is a medical condition characterized by an abnormal accumulation of fluid in the pleural space, which is the area between the lungs and the chest wall. The pleura is a bilayered membrane that surrounds the lungs, allowing them to expand and contract smoothly during breathing. Under normal conditions, a small amount of pleural fluid (about 10-20 ml) is present to facilitate lung movement. However, when this fluid accumulates beyond the normal physiological amount, it leads to pleural effusion.
Pleural effusion is a significant medical concern and can be caused by various underlying conditions, including infections, heart disease, malignancies, and systemic illnesses. In India, tuberculosis (TB) remains one of the most common causes of pleural effusion due to its high prevalence.
Causes of Pleural Effusion
Pleural effusion can result from multiple medical conditions, broadly classified into transudative and exudative effusions.
1. Transudative Pleural Effusion:
Occurs due to imbalances in hydrostatic and oncotic pressure without significant inflammation. Common causes include:
- Congestive Heart Failure (CHF): The most common global cause of transudative pleural effusion.
- Liver Cirrhosis: Due to decreased albumin production leading to fluid leakage.
- Renal Failure (Nephrotic Syndrome): Causes low protein levels, resulting in fluid accumulation.
- Hypoalbuminemia: A deficiency of albumin leading to fluid imbalance.
2. Exudative Pleural Effusion:
Occurs due to increased capillary permeability and inflammation. Common causes include:
- Tuberculosis (TB): One of the leading causes in India, accounting for a significant number of pleural effusion cases.
- Pneumonia and Lung Infections: Bacterial, viral, or fungal lung infections can cause inflammation and fluid accumulation.
- Malignancy (Cancer): Lung cancer, breast cancer, and metastatic cancers can lead to recurrent pleural effusions.
- Pulmonary Infarction: Blood clot in the lungs (pulmonary embolism) can cause fluid buildup.
- Lymphatic Disorders: Blockage of lymphatic drainage can lead to chylous effusion.
- Connective Tissue Diseases: Conditions like rheumatoid arthritis and lupus can cause pleural inflammation.
- Post-Surgical or Post-Traumatic Causes: Following lung surgeries, chest trauma, or radiation therapy.
Symptoms of Pleural Effusion
The severity of symptoms depends on the amount of fluid accumulated and the underlying cause. Common symptoms include:
- Chest pain (worsens on deep inspiration or coughing)
- Shortness of breath (Dyspnea) – can be mild or severe depending on fluid accumulation.
- Fever and chills – especially in infectious causes like pneumonia and tuberculosis.
- Weight loss – commonly seen in malignancies and TB-related effusion.
- Persistent cough – sometimes associated with blood-tinged sputum in malignancies.
- Fatigue and weakness – due to reduced lung function and underlying chronic disease.
Diagnosis of Pleural Effusion
A timely and accurate diagnosis is crucial for determining the cause of pleural effusion and guiding treatment.
1. Ultrasound of the Chest:
- The most sensitive and earliest method to detect pleural effusion.
- Can detect even 10 ml of fluid and localize the exact site for fluid sampling.
- Helps identify septations, loculated fluid, and pleural thickening.
2. Chest X-ray (CXR):
- A commonly used imaging technique.
- Detects pleural effusion when fluid volume is above 200-300 ml.
- Features like blunting of costophrenic angle, mediastinal shift, and layering fluid help in assessment.
3. Computed Tomography (CT) Scan:
- Provides a detailed view of the lungs and pleural space.
- Useful in detecting malignancies, pleural thickening, and associated lung pathologies.
4. Pleural Fluid Analysis (Thoracentesis):
- Gold standard for diagnosing pleural effusion.
- A bedside procedure where a needle is inserted into the pleural cavity under ultrasound guidance.
- Fluid is aspirated and sent for biochemical, microbiological, and cytological analysis.
Pleural Fluid Analysis Tests Include:
- Protein and LDH levels: To differentiate transudative vs. exudative effusion (Light’s Criteria).
- Glucose levels: Low in infections and malignancies.
- ADA (Adenosine Deaminase): High in tuberculosis-related pleural effusion.
- Gram stain and cultures: To detect bacterial infections.
- Cytology: Helps detect malignant cells in cancer-related effusions.
Treatment of Pleural Effusion
The treatment approach depends on the underlying cause of the pleural effusion.
1. Medical Management:
- Antibiotics: For bacterial infections like pneumonia.
- Anti-tubercular Therapy (ATT): If pleural effusion is due to tuberculosis (common in India).
- Diuretics: Used in cases of cardiac failure to remove excess fluid.
- Immunosuppressants: Used for autoimmune conditions like lupus and rheumatoid arthritis.
2. Therapeutic Thoracentesis:
- Performed when there is significant fluid accumulation causing breathing difficulty.
- Up to 2 liters of fluid can be removed in one sitting to relieve symptoms.
3. Chest Tube Drainage (Intercostal Drainage – ICD):
- Used in recurrent or large pleural effusions.
- A tube is inserted into the pleural cavity to continuously drain the fluid.
4. Pleurodesis:
- A procedure used for recurrent malignant pleural effusions.
- Chemical agents like talc are introduced into the pleural space to adhere the pleura together, preventing further fluid accumulation.
5. Surgery (Video-Assisted Thoracoscopic Surgery – VATS):
- Used in complicated cases like empyema (infected pleural effusion) or malignancies.
- Allows direct visualization and biopsy collection.
Complications of Pleural Effusion
If left untreated, pleural effusion can lead to severe complications, including:
- Lung Collapse (Atelectasis): Due to increased pressure from fluid accumulation.
- Empyema: Pus formation in the pleural cavity, requiring surgical drainage.
- Fibrosis and Scarring: Chronic inflammation leading to restrictive lung disease.
- Respiratory Failure: In cases of severe or recurrent effusions.
Conclusion
Pleural effusion is a serious medical condition requiring prompt diagnosis and appropriate treatment. In India, tuberculosis remains a major cause, making early detection through ultrasound and pleural fluid analysis crucial. A multidisciplinary approach involving pulmonologists, radiologists, and infectious disease specialists is essential for effective management.
For individuals experiencing persistent breathlessness, chest pain, or unexplained weight loss, seeking medical evaluation is critical. Timely intervention can prevent complications and improve outcomes in pleural effusion cases.